|
|
 |
 |
 |
Of all the neurotransmitters and hormones
that may be involved in depression, serotonin and the hormones of the hypothalamic-pituitary-adrenal (HPA)
axis probably play the most important role. They also appear
to share certain physiological pathways, which would keep
them interacting constantly. The recent consensus that the hippocampus,
a structure in the limbic system, also forms an integral part
of this “stress axis” has provided a better overall
understanding of the complex phenomenon of depression.
It is thus becoming increasingly obvious that hyperactivity in the stress axis is not just a side-effect of depression. The stress axis and the serotonergic systeminteract in many ways. These interactions are probably among the reasons that the level of glucocorticoids circulating in someone's body greatly affects their mood, partly because of their effects on the hippocampus.
Long associated with cognitive processing of information, and with memory in particular, the hippocampus has more recently been recognized as an integral part of the circuits that control our moods and emotions. The fact that depressed patients often have a variety of memory deficits also points toward the involvement of the hippocampus in depression. |
Epileptic seizures that are focused in the temporal lobe produce massive loss of neurons in the hippocampus and neighbouring structures. In patients with epilepsy, depression is the most common psychiatric complication,
and patients with temporal lobe seizures are more likely to suffer from depression than patients with other forms of epilepsy.
These observations thus strongly suggest a link between depression and damage to the hippocampus. |
|
|
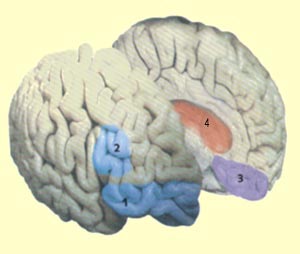
| PARTS OF THE BRAIN THAT SLOW DOWN OR SPEED UP IN DEPRESSION |
|
Though depression involves an
overall reduction in brain activity, some parts of the brain
are more affected than others. In brain-imaging studies using PET
scans, depressed people display abnormally low activity in the prefrontal
cortex, and more specifically in its lateral, orbitofrontal,
and ventromedial regions.
And the severity of the depression often correlates with the extent
of the decline in activity in the prefrontal cortex.
| The prefrontal
cortex is known not only to be involved in emotional responses,
but also to have numerous connections with other parts of the
brain that are responsible for controlling dopamine,
norepinephrine, and serotonin, three neurotransmitters
that are important in mood regulation. More specifically, the lateral prefrontal
cortex seems to help us choose a course of behaviour
by letting us assess the various alternatives mentally. The orbitofrontal cortex seems
to let us defer certain immediate gratifications and suppress
certain emotions in order to obtain greater long-term benefits.
And the ventromedial cortex is thought to
be one of the sites in the brain where we experience emotions
and the meanings of things. |
|
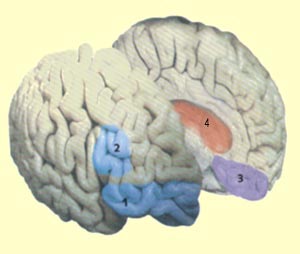
1) orbitofrontal cortex
2) lateral prefrontal cortex
3) ventromedial cortex
4) limbic system |
The two halves of the prefrontal cortex also seem to have specialized
functions, with the left half being involved in establishing positive
feelings and the right half in establishing negative ones. And
indeed, in depressed people, it is the left prefrontal cortex that
shows the greatest signs of weakness. In other words, when people
are depressed, they find it very hard not only to set goals in
order to obtain rewards, but also to believe that such goals can
be achieved.
In healthy people, the left prefrontal cortex might also help to inhibit the
negative emotions generated by limbic structures such as the amygdalae, which
show abnormally high activity in depressed patients. In patients who respond
positively to antidepressants, this overactivity is reduced. And when the amygdalae
remain highly hyperactive despite antidepressant treatment, the likelihood of
a patient's relapsing into depression is high.
It is also interesting to note that when someone's left prefrontal cortex is
operating at full capacity, the levels of glucocorticoids in their blood are
generally very low. This follows logically, considering the
harmful effects that high levels of glucocorticoids have on mood.
Brain-imaging studies have also shown that in patients with severe depression,
the volume of the two hippocampi is
reduced. This atrophy may be due to a loss
of neurons that is also induced by the toxic effects of the high levels of
glucocorticoids associated with recurrent episodes of depression.The extent of
atrophy in the hippocampus even seems to be proportional to the sum of the durations
of the episodes of depression, and depressions that are treated rapidly do not
seem to lead to this reduction in hippocampal volume (see sidebars).
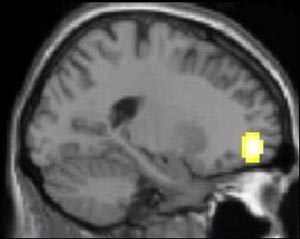
In
an experiment using functional magnetic resonance imaging
(fMRI), a group of healthy people and a group of depressed
people were shown clips from sad films. Both groups were
asked to try to suppress any feelings of sadness that the
films elicited.
The image here represents the arithmetical difference between
the brain activity levels of healthy subjects and of depressed
subjects. It shows that the healthy subjects had more activity
in the lateral portion of the orbitofrontal cortex (Brodmann
area 11), which plays a major role in regulating emotions.
This is not surprising: since depressed people have a lot of
trouble in inhibiting their negative emotions, it makes sense
that their orbitofrontal cortexes would be less active than
those of healthy people.

|
|
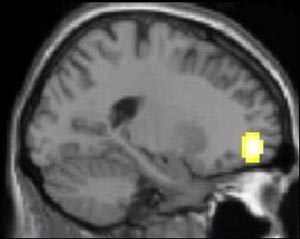
Source: Mario Beauregard, Centre
de recherche de l'Institut universitaire de gériatrie
de Montréal |
Why would evolution have
allowed the human brain to develop and maintain circuits
that can cause depression? Some potential answers can be
found in the animal kingdom. When an animal is faced with
a disagreeable situation and can neither fight nor flee,
it responds with inhibition
of action, a state that resembles depression.
The status of the most subordinate animals in a hierarchy
may also have an adaptive value, by preventing them from
engaging in fights that could be very costly, or even fatal.
This would also explain why in human beings today, depression
is often triggered by events that undermine self-confidence—the
equivalent of being defeated by a more dominant animal. |
|
|