|
|
Walking
in Nature Stops You from Brooding
One possible interpretation
of certain brain-imaging studies is that in depression, a
vicious cycle becomes established among various structures
of the limbic system that have become hyperactive.
We already know that all of these structures are interconnected
by neural pathways. Thus someone's amygdala,
which can generate a
number of emotions related to fear, might produce a negative
emotion, the prefrontal lobes would revive
some bad memories associated with this emotion, the anterior
cingulate cortex would prevent the person from thinking
of anything else, and the thalamus would promote
the activity of the circuits that form this “depression
loop”. |
A substantial reduction
in the number of glial
cells in certain parts of the brain, such as the ventromedial
prefrontal cortex, has been observed in people who are clinically
depressed.
This discovery is interesting, because it might explain some
other observations associated with depression, such as atrophy
or a decline in neural activity in certain parts of the brain.
The function of certain glial cells, such as astrocytes,
is to supply the neurons with energy. Hence, if the number
of astrocytes decreased, a decline in the activity of the associated
neurons could be expected.
|
|
|
| PARTS OF THE BRAIN
THAT SLOW DOWN OR SPEED UP IN DEPRESSION |
|
One of the regions of the prefrontal
cortex that is most affected both by depression and by
the manic phase of manic depression is the ventromedial
cortex (also known as the subgenual cortex, because
it sits beneath the genua, or knee, of the corpus callosum).
This area deep inside the frontal lobes, on either side of
the centre line separating the two hemispheres, lets us switch
from one kind of affect to another. It is also heavily involved
in feelings
of pleasure and positive reinforcement.
The ventromedial cortex has very dense connections with the limbic
system. These connections make the ventromedial cortex an ideal
structure for linking the conscious to the unconscious and for
ascribing meaning to perceptions by associating them with a meaningful
whole. Also, this region is strongly modulated by the neurotransmitters
involved in depression.
Studies
of people with a family form of depression or manic depression
have shown that the ventromedial cortex was up to 40% smaller
in people who were clinically depressed. When researchers
investigated what might be happening at the cellular level
to account for this atrophy in this part of the brain, they
found that it was not the number of neurons that had diminished,
but rather the number of glial cells that had fallen drastically
(see sidebar).
Several experiments have shown that, like many other parts
of the prefrontal cortex, this “emotional control centre” is
nearly inactive during the depressive phase of manic depression,
but becomes hyperactive during the manic phase. The logic
of these two opposite states can also be observed in certain
symptoms. For example, people in a manic phase find meaning
in everything they do, whereas people who are depressed experience
an overall loss of meaning in their lives. |
|

1) orbitofrontal cortex
2) lateral prefrontal cortex
3) ventromedial cortex
4) limbic system
5) anterior cingulate cortex |
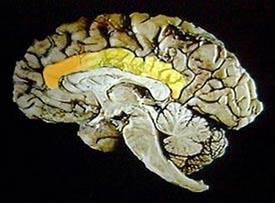
The cingulate cortex is
another brain structure that seems to be involved in depression.
This part of the cortex is very old in evolutionary terms. It lies
along numerous
pathways ascending from the unconscious, emotional limbic brain,
as well as other pathways that descend from the conscious, prefrontal
cortex and that are involved in planning actions.
The cingulate cortex has been observed to be less active in people
who are depressed and hyperactive in people who are manic. But
the anterior portion of the cingulate cortex, unlike the rest of
this structure, becomes more active during depression. Though the
functions of the anterior cingulate cortex (or gyrus) are highly
complex, it seems to act somewhat like an interface between the
lower, more instinctive parts of the brain and the more rational
circuits of the neocortex. In healthy people, the activation of
this structure would thus help to focus attention on certain phenomena,
often arising from our own bodies, such as pain, or the negative
feelings associated with depression.
The cingulate cortex (yellow) and its anterior portion
(orange) in a sagittal section of the brain |
|
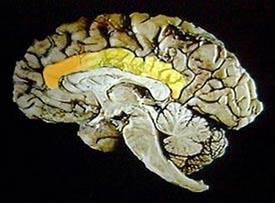
Source: Suzanne Stensaas and O.E.
Millhouse, The Digital Slice of Life |
Norepinephrine plays
a role in the functioning of the body's alarm system, through
the sympathetic
nervous system and the hypothalamic-pituitary-adrenal
(HPA) axis. But norepinephrine's exact role in depression
remains ambiguous. On the one hand, a decline in the activity
of the serotonergic or norepinephrinergic circuits appears
to favour the onset of a depressive state. But on the other
hand, some studies report the opposite: hyperactivity in
the norepinephrinergic system during depression.
Autopsies have shown, however, that patients who had experienced
multiple depressive episodes had fewer norepinephrinergic neurons.
A large part of the problem may therefore be the ability or
inability of the norepinephrinergic system to respond properly
to the demands of stress. As research increasingly shows, negative
experiences with parental care in early life have an important
impact on an individual's ability to manage stress as an adult.
These experiences might have persistent effects on several
systems, including the norepinephrinergic system.
|
|
|